When I was working in the sterile pharmaceutical industry, I reviewed the The Australian Code of Good Manufacturing Practice for Medicinal Products (2002) as part of my self-development. This code was revoked effective from 1 July 2010 and replaced by the PICS Guide for Good Manufacturing Practice for Medicinal Products 2009, as adopted in Therapeutic Goods (Manufacturing Principles) Determination No. 1 of 2009. Here’s the original review.
I have now reviewed the PICS Guide for Good Manufacturing Practice for Medicinal Products 2009, from the stand point of a microbiologist working collaboratively in a sterile pharma plant. What my review does is make note of the salient points and I add comments to some.
Both the revoked 2002 Australian GMP code and the 2009 PICs guide are based on ICH Q&A Good Manufacturing practice Guide for Active Pharmaceutical Ingredients which was last modified in 2000. In 2015 21 pages worth of clarifications were published to clear up some technical questions and to remove ambiguities. Looking at them, I’m not sure why clarification was needed as they all seem straight forward and answerable by anyone experienced working within a pharmaceutical manufacturing environment. This means that despite having “no recent experience” as deemed by some potential employers, my knowledge is still bang up to date. Combine that with my fantastic memory and impressive technical skills and I’d be an asset to your company.
Italics show my comments.
The PIC/S guide to GMP for medicinal products – click here to be taken to the PIC/S website (opens in new window)
CHAPTER 1 – Quality Management
Principle
- Manufacturers must ensure products are fit for their intended use and do not put patients at risk due to inadequate safety, quality of efficacy. This is the responsibility of senior management. >>a robust Quality Management System (QMS) needs to be in place.
Quality Assurance (QA)
- QA’s anything that influences the quality of a product.
- Products made using Good Manufacturing Process (GMP)
- Everything is documented and validated
- Responsibilities are clearly stated
- Products cannot be sold until approved (or at least certified it was produced and controlled properly) for release >>interesting if someone’s placed an order
- Suitable product storage needs to be in place >>stability studies would support the stated storage conditions
- An internal audit system needs to be in place
GMP For Medicinal Products
- Concerned with both production and quality Control (QC)
- Processes to be clearly defined, systematically reviewed and shown to produce a consistent output within specifications
- Critical steps and critical changes to be validated >>here you’d want to explain why one step is deemed critical while another is not
- >>Pretty much a statement as to the 5/10ths of the commandments of GMP is next
- Written instructions to be clear and unambiguous >>so things are reproducible and not open to interpretation.
- Operators need to be trained >>and certified competent
- Records need to be made as it happens and ‘significant’ deviations need to be recorded and investigated. >>immediate investigation where necessary, possibly via scheduled sterile media trials
- Batch tracing is required >>allows investigation on adverse events or product recalls
- Product complaints need investigation and if necessary corrective and preventative action (CAPA) put in place
Quality Control
- Concerned with sampling, specs and testing, with documentation and procedures ensuring testing is carried out properly so release product is deemed satisfactory >>i.e. unadulterated and regulatory compliant
- >>Pretty much a statement as to the 5/10ths of the commandments of GMP is next
- Sampling needs to be done by personal and methods approved by QC
- Test methods need to be validated
- Same deal with recording data as for GMP section
- Enough samples of starting materials and finished product need to be retained in final packaging for future examination >>I was not aware of the starter material requirement. Good to know
Product Quality Review
- Regular (or rolling) review needed to show product consistency, identify trends, appropriateness of specs, and identify improvements. Needs to consider previous reviews. >>These are your Annual Product Reviews
- 12 specifics follow.
- CAPA needs to be examined for effectiveness.
- If using contract manufacturers, who is responsible for what needs to be documented.
Quality Risk Management
- Can be proactive or retrospective and covers the assessment, control, communication and review of quality risks to the product
- The Quality Risk Management System (QRMS) needs to be scientifically sound and consider the patient.
- The amount of effort put into this to be based on the level of risk >>using risk assessment/evaluation tables incorporated into your Risk Assessment procedure is the way to go
- Reference made to Annex 20 – Quality Risk Management <insert link?>
CHAPTER 2 – Personnel
Principle
- Basically QA and the correct manufacture of product relies on people. Responsibilities need to be stated, everyone needs to be aware of GMP and everyone needs to be trained (and retrained).
General
- Enough qualified and experienced people need to be employed and individuals should not be overloaded (if it impacts quality)
- You need an organizational chart with the responsible people having specific duties recorded. Gaps or overlaps are not allowed when it comes to the application of GMP.
- Key Personnel
- Production and QC heads. Product release head (if the other two are not responsible for it. >> unless thing have changed, I was taught QA should sit above QC and Production and be responsible for release.
- Key roles to be full time (normally) and independent of each other. Delegation of responsibility is allowed.
- Responsibilities of each key role are listed. Additional QC Dept roles in Chapter 6.
Training
- Appropriate training required for all.
- Basic GMP training for all, with specific training relevant to task performed with periodic assessment. Approved training programs to be used. >>if it was not documented, it never happened.
- Visitors to be kept out of QC areas, unless unavoidable and then closely supervised >>some auditors want in to production clean rooms, no matter what.
- QA should be fully discussed along with GMP in training
Personal Hygiene
- Hygiene programs are to be detailed and dependent on need. Should also relate to health, hygiene and clothing of personnel. Should ne understood and strictly adhered to. Programs should be promoted by management,
- Medical exam upon recruitment and then whenever necessary to ensure work and personal health.
- Nobody with an exposed lesions or an infectious disease should be used to manufacture product. >> cuts, weeping wounds, cold or flu? Assign them to other duties, otherwise they’ll be shedding particles all over your nice clean production facility
- Protective garments to be worn appropriate to operations >>protection for self and for product
- Eating or storing food in production and storage areas is prohibited, as is smoking. Any unhygienic practice that could affect product should also be forbidden.
- Direct contact with filling surfaces and hands should not happen >>presumably this means with or without gloves
- Personal should be instructed to use the hand washing facilities >>don’t instruct, enforce!
CHAPTER 3 – Premises and Equipment
Principle
- Design and build your plant to suit the operations. Layout should permit effective cleaning and maintenance and minimize error risk and cross contamination so product quality is not adversely affected
Premises – General
- Site the premises to minimize risk of contamination of materials or products >>geographically? Not next to a coal plant? Here as long as your site has appropriate airlocks, filers, is not in a swamp or next to a dump, you are probably safe.
- Maintain and clean the facility according to written procedures.
- Maintain the environment carefully to not adversely affect product manufacture or storage and so equipment functions within specification
- Premises to be as insect and animal proof as possible.
- Access control is needed to keep unauthorized people out. >>both employees using “short cuts to the canteen” and strangers off the street.
Premises – Production Area
- Segregate various classes of product production (eg cytotocics, penicillins, live preparations (in a sterile facility??) using dedicated self-contained facilities. Should not (DO NOT) manufacture technical poisons in premises used for medicinal products. >>not even same site. Risk of disaster if cross contamination huge.
- A logical production layout is advised as is logical positioning of equipment in order to reduce confusion and the introductions of errors (that would affect product quality). Emphasized again in 3.15
- Rooms to be non-shedding and easy to clean, pipes, conduits etc to be recess free and easy to clean and preferably easy to access from outside production >> I’ve crawled through roof spaces to access the other side of airlock ventilation ducts. Probably need a confined space permit for that these days.
- Drains to have trapped gullies and preferably avoid open channels.
- Production to be environmentally controlled
- Stating material to be weighed in separate weighing room >>I’ve seen starting material weighed in alcove in mixing rooms – justification would be needed
- Where dust is produced, specific anti cross contamination provisions needed >>eg extraction hood and curtains as was the case in point above.
Premises – Storage Area
- Storage areas should be large enough and designed to be fit for purpose and maintained
- Quarantine areas to be clearly marked and access restricted
- Sampling of starting materials should be conducted to prevent cross contamination
- Rejected materials to be stored separately
- Highly active material to be stored in safe secure areas >>Material to be stored according to hazardous material regulations etc.
- Critical packaging material with regards to conformity of products, to be stored safely and securely
Premises – QC Areas
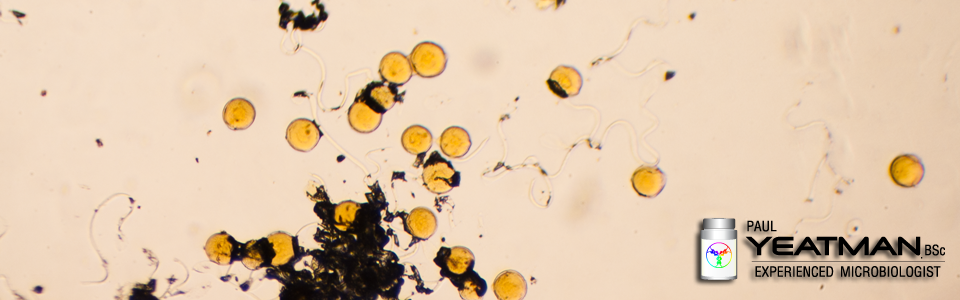
- Normally separated from production, esp. important where there’s a microbiology lab with viable organisms kicking about
- Suitable design so fit for purpose with enough space and minimal risk of mix-ups
Premises – Ancillary Areas
- Rest/refreshment areas separated from other areas
- Change rooms and toilets to be easily accessible and fit for user numbers. Toilets not to directly link to production or storage areas.
- Maintenance to be as far as possible from production areas. Tools and parts kept in lockers reserved for such use.
- Animal houses to be isolated with dedicated animal entrance and separate air handling.
Equipment
- Manufacturing equip fit for purpose and easily cleaned, according to documented, validated procedures and to be stored clean and dry
- Repair and maintenance operation not to risk product quality
- Washing and cleaning equip (to be chosen to) not to be a source of contamination >>chemical, particle or microbiological
- Product contact production equipment to be non-reactive additive or absorptive – cannot affect the product or introduce hazards
- Measuring equipment to be validated and calibrated and fit for purpose and records kept
- Fixed pipework to be labelled showing direction of flow
- WFI, Purified Water systems etc to be sanitized according to written procedures with stated microbiological action limits and what to do when breached
- Defective equipment to be clearly labelled, and preferably relocated from production >>if it is still there you can guarantee someone will use it despite all their training retraining
CHAPTER 4 – Documentation
Principle
- Essential part of QA.
General
- Explanation of what type of docco is what.
- Doccos should comply with regs and should not be slipshod
- Doccos need dated approvals by authorized persons
- Doccos need to be unambiguous in content and title and regularly reviewed with copies being legible
- The only hand written content is recorded data, which must be made in indelible ink with alterations annotated and the oriental data legible
- Data to be recorded AS IT HAPPENS, not at a later date and retained +1 year after product expiry
- Record data any way you want, but make sure the process is fully documented and checked for accuracy with data modification limited to authorized personnel. If using electronic records, BACKUP! Data to be readily available during retention period
Documents Required – Specifications
- Should be authorized and dated for everything , inc. if appropriate, intermediate and bulk products
- Details of what the specs should include
Manufacturing formula and processing instructions
- Recipes for each product and batch size should exist and be approved
- Details of what should be in what docco is then stated.
Packaging Instructions
- Same deal as formula and processing
Batch Processing Records
- Each batch should have a complete manufacturing record with all required details on which data is recorded as it happens and by whom. Certain steps need to be approved before the batch is authorized to begin
Batch Packaging Records
- Same deal as for processing records
Procedures and Records – Receipt, Sampling & Testing
- Written records of what is done with what and by whom is needed
Procedures and Records – Other
- Release and rejection procedures needed and appropriate signatures required and documentation retained on batch distribution in the event that a recall is required.
- Specifies what needs written procedures and records of actions taken or conclusions reached
- Clear OI’s for major items of manufacturing and test equipment >>eh? Everything needs that!
- Log books needed for all major or critical equipment and need to be filled in correctly >>if it’s non critical equipment, how do you know if it was within calibration or even used? See above point.
CHAPTER 5 – Production
Principle
- GMP needs to be complied with and defined regulatory compliant procedures followed
General
- Operators need to be competent as do supervisors
- Written procedures to be followed
- Details of how to handle incoming materials, intermediate and bulk product
- Operate in such a way as to reduce cross contamination risk (esp. microbiological)
- Reduce dust generation
- Label rooms with the batch they are making at the time >>also cleaning status if not in use
- Transfer lines should be checked for correct setup
- Avoid deviating from written procedures and if so get approval (documented) from QC when appropriate >>your written procedures should tell you when you can make the call yourself
- Restrict access to facility
- Avoid making non medicines with areas and equip intended for medicinal production
Prevention of Cross-Contamination in Production
- This must be avoided. Details on how to avoid are provided. Any measures taken should be checked for effectiveness periodically.
Validation
- Studies should reinforce GMP. Results and conclusions to be recorded >>obviously!
- If it is new, validate it, if it is an amendment, validate it, if it is for like for like, prove it.
- Periodically reassess
Starting Materials
- Only acquired from approved vendors >>who have been audited by your QA dept
- Details on testing, storage and labeling are stated
- Only use approved and release materials
- Dispensed material needs independent checking of weights or volumes
Processing Operations – Intermediate and Bulk Products
- Line clearances should be performed between batches
- Critical processes should be validated and the process (incl. deviations) recorded and the method/SOP/OI followed
Packaging Materials
- Same deal as with stating materials
- Outdated or obsolete primary packing should be destroyed and such destruction recorded
Packaging Operations
- Minimization of cross contamination emphasized again – recurring theme
- Very similar to processing operations
- More extensive requirements than for filling >>makes sure the items are correct labelled and packaged so Anzatax is not labelled and boxed up as Morphine for example
- Batch reconciliation should be performed. >>filled 100 000 vials. Packaged 99500, probably ok. Missing 5000 units, probably not. Some products like Drugs of Addiction need closer attention due to other Government regulations.
Finished Products
- Quarantine until al testing shows fit for release (and if not, onto the next section…)
Rejected, Recovered and Returned Materials
- Rejects to be clearly marked. Appropriate (documented) action to be taken
- Reprocessing not advised.
- Any recovery procedures to be pre authorized and documented and the need for further testing considered by QC
- If product is returned form the market, it should be destroyed. >>unknown history. Pretty much a case of if in doubt, throw it out. PIC/s say QC has the final say. I’d want QA to do that.
CHAPTER 6 – Quality Control
Principle
- Concerned with sampling and testing, organization, documentation and release procedures to ensure everything is done as it should be. Must be independent from Production – considered fundamental. >>In the past, in my experience, QC’s been at the lab level and QA’s at the audit, QMS and release level and stood above QC. QC make sure everything is done according to spec and is reactive. QA makes sure everything is up to by the book and is proactive.
General
- Should be separate from all other departments and staffed with an appropriate number of appropriately qualified persons
- Chapter 2 summarizes the QC head’s principal duties.
- QC Dept to establish, validate and implement all QC procedures to ensure everything happens to established regulatory compliant procedures
- QC should have access to production for sampling and investigative activities
Good QC Lab Practice (GLP)
- Should meet the Chapter 3 requirements.
- Everything should be appropriate for the task performed and if using a contract lab, refer to Chapter 7
Documentation
- Should follow Chapter 4 principles.
- Should be readily available >>otherwise how are staff to know how to test what according to what and what the specs are?
- Batch record related doccos to be retained +1 year on expiry
- Records of kept in form that allows trending >>conduct trending on a regular schedule – 3-6 months with a QA review/report submission every 12
- Original data should be readily available during retention period
Sampling
- According to documented procedure
- Reference samples should be representative of batch >>of course
- Reference samples should be kept +1 year on expiry. Finished goods in original packaging. Starting material should be kept for 2 years (is stability allows). Keep enough to allow full retesting.
Testing
- Analytical methods should be validated
- Results should be recorded and checked (for consistency). Calculations to be critically examined >>if auto calculated, make sure the software or spreadsheet is validated
- Details of data to record stated
- The need to record, to label to follow written procedure emphasized
On-Going Stability Program
- Monitor product over course of shelf life to ensure product efficacy remains (and strange product things do not happen, such as dissolution, or loss of preservative function etc)
- Program needs to be documented
- What the program should include is listed
- Enough testing (numbers and test points) for trend generation should be done.
- Data should be available to key personnel and auditors/reg authorities
- Out of specs to be investigated >>obviously
- Summary should be maintained and periodically reviewed >>are the results of batch a similar to batch B, C, D and are we seeing any adverse trends, etc.
CHAPTER 7 – Contract Manufacture and Analysis
Principle
- What happens needs to be documented and agreements need to be in place between Contract Giver and Contract Acceptor
General
- Written contract and if any changes to analysis proposed, must be in accordance with marketing authorization
The Contract Giver
- Responsible for assessing competence of Contract Acceptor
- Should provide contract lab with all info needed to carry out the contracted out work, including any safety information
- Should ensure everything provided from Contract Acceptor is up to spec.
The Contract Acceptor
- Same deal as to site design, equipment, training, etc as for any GMP facility
- Should make sure what they receive if fit for purpose
- Cannot sub contract work unless preapproved by Contract Giver
- Should refrain from anything that might adversely affect product quality >>so follow GMP and GLP
The Contract
- Should be drawn up by someone competent and state who does what, when, where and with what and be signed off by both parties.
- Same requires for retention of samples/data as per Contract Giver
- Contract should allow for onsite audits by Contract Giver
- Contract Acceptor should also be aware that the reg authorities can audit them as well
CHAPTER 8 – Complaints and Product Recall
Principle
- All complaints should be reviewed according to written procedures and a recall system should be in place
Complaints
- A product complaint role should have a dedicated person. If it’s not a QA/QC Dept head, they should be made aware of the complaint
- Follow written procedures and record details, including findings
- If product defect discovered (or suspected), consider investigating related batches >>eg delamination of shell glass vials? Any other batches affected using same batch fo vials (or supplier?)
- Review complains regularly as trends may be shown >>at annual product review would be a good time
- Mention of counterfeits and if that is why there was a complaint.
- Need to notify authorities if major issue >>eg if a recall is likely
Recalls
- Dedicate someone to handle recalls, preferably independent of sales and marketing. If it’s not a QA/QC Dept head, they should be made aware
- Follow written procedures, record everything
- Should be able to recall at the drop of a hat.
- Authorities in countries where product’s been shipped should be informed prompt as should the customers
- Recalled product to be stored on site separately until fate decided
- Regularly evaluate effectiveness of recalls >>one would hope there would not be many recalls to review
- Though not mentioned, performing a batch reconciliation would be a good idea on the returned samples
CHAPTER 9 – Self Inspection
Principle
- Should be done to make sure things are happening as they should and to propose CAPA where they are not
- Basically everything in Chapters 1-8 should be inspected for compliance
- Should be done independently by designated competent persons. Can use external auditors >>i.e. if it if your own department, don’t audit your processes. while working in the microbiology lab, I’d audit production processes.
- Document the process and findings. IF CAPA, follow action to be recorded. >>and presumably closed out
Annex 1 – Manufacture of sterile medicinal products
No review is required here. PIC/S summarizes the interpretations an inspector adopts during an audit. It is a good idea to have answers to why you do the things the way you do them if the guidelines suggest you should do things another way. As always, whatever way you do things, the justification needs to be documented in the form of policies or validations and approved by the Quality Assurance representative.
Did you find this informative or useful? Please consider a small donation so I can expand and improve on what I deliver.
![]()